Urology
What is Balanitis and How Is It Treated?

by admin
17th October 2023
7 minutes read
Introduction
The word Balanitis might not be very familiar to most of you. However, it is a common and uncomfortable condition that affects men. It results in inflammation of the glans penis or the head of the penis. It might be commonly referred to as “penis infection” or “penile infection”. Balanitis is caused by lack of hygiene in most of the cases and it can be recurrent if not taken adequate care. In this blog let’s understand balanitis in detail and how it is treated.
What is Balanitis?
Balanitis is a medical condition characterized by the inflammation of the glans penis, which is the rounded tip of the male genital organ. It is often accompanied by redness, swelling, and irritation of the glans penis and can cause symptoms such as itching, pain, and, in some cases, the presence of discharge. Balanitis can result from poor hygiene, bacterial or fungal infections, exposure to any allergens or irritants, or any skin conditions such as psoriasis or eczema. Balanitis can cause discomfort and may affect a person’s quality of life. Treatment for balanitis typically involves addressing the underlying cause.
Symptoms of Balanitis
The symptoms of balanitis typically include the following:
- Redness: The glans penis (the rounded tip of the penis) becomes red and inflamed.
- Swelling: Swelling or edema of the glans penis may be noticeable.
- Itching: Itchiness in the genital area, particularly around the glans penis, is a common symptom.
- Irritation: The affected area may feel sore or irritated.
- Pain: Balanitis can cause discomfort or pain in the penis, particularly when urinating or during sexual activity.
- Discharge: Some individuals may experience discharge, which can be white, yellow, or greenish in color and may have an unpleasant odor.
- Difficulty retracting the foreskin: In cases where the foreskin is involved, it may become difficult to retract it over the glans penis.
- Cracking or fissures: In some cases, the skin of the glans penis may develop small cracks or fissures.
It’s important to note that these symptoms can result from various causes of balanitis, including infections (bacterial or fungal), skin conditions, poor hygiene, or exposure to irritants or allergens. If you experience any of these symptoms, especially if they persist or worsen, it’s advisable to seek medical attention. A healthcare professional can diagnose the underlying cause of the balanitis and recommend appropriate treatment to alleviate the symptoms and prevent complications.
How is Balanitis Diagnosed?
Balanitis is typically diagnosed through a combination of medical history, physical examination, and sometimes laboratory tests. Here’s how the diagnosis of balanitis is usually conducted:
- Medical History: The healthcare provider will begin by discussing your medical history and asking questions about your symptoms. This may include inquiries about the onset, duration, and progression of symptoms, as well as your sexual history and hygiene practices.
- Physical Examination: A thorough physical examination will be conducted, focusing on the genital area. The healthcare provider will inspect the glans penis for signs of redness, swelling, discharge, or other abnormalities.
- Laboratory Tests: In some cases, especially when the cause is unclear, laboratory tests may be necessary. These can include:
- Swab Culture: A sample may be taken from the affected area to identify the specific pathogen causing the infection, whether it’s bacteria or fungi.
- Blood Tests: These tests can be used to check for underlying conditions, such as diabetes or sexually transmitted infections (STIs), which can contribute to balanitis.
- Skin Biopsy: In rare and challenging cases, a small sample of skin may be taken for a biopsy to determine the underlying cause, especially when conditions like psoriasis or lichen sclerosus are suspected.
The diagnosis of balanitis aims to identify the underlying cause, whether it’s an infection, skin condition, irritant, or allergy. Once the cause is determined, appropriate treatment can be recommended. If you suspect you have balanitis or are experiencing symptoms, it’s crucial to consult a healthcare professional for an accurate diagnosis and tailored treatment plan.
Treatment For Balanitis
The treatment for balanitis depends on the underlying cause. Here are some common treatment approaches:
- Oral Medications: In more severe or persistent cases, oral antibiotics or antifungal medications may be prescribed to address the infection.
- Circumcision: In cases of recurrent or severe balanitis, especially when caused by phimosis (tight foreskin), circumcision may be recommended. This surgical procedure removes the foreskin.
- Treatment of Underlying Conditions: If an underlying medical condition, such as diabetes or a skin disorder, is contributing to balanitis, treating that condition is essential.
- Lifestyle Changes: Avoiding potential irritants, maintaining good personal hygiene, and using protection during sexual activity can help prevent future episodes.
It’s crucial to seek medical advice if you suspect you have balanitis, as the cause and appropriate treatment can vary. Avoid self-diagnosis and self-treatment, as they may worsen the condition or lead to complications.
5 Preventive Measures for Balanitis
Preventive measures for balanitis aim to reduce the risk of inflammation and infection of the glans penis. Here are five key steps to help prevent balanitis:
1. Practice Good Hygiene:
Gently clean the genital area, including the glans and, if applicable, the foreskin, daily with warm water. Avoid using harsh soaps or irritants, as they can exacerbate the condition.
2. Avoid Irritants:
Steer clear of using harsh soaps, detergents, or perfumed products in the genital area, as they can cause irritation. Use mild, hypoallergenic soaps if necessary.
3. Keep the Genital Area Dry:
After washing, make sure to thoroughly dry the genital area, including under the foreskin if it is present. Excess moisture can promote fungal growth, a common cause of balanitis.
4. Use Condoms:
Practicing safe sex and using condoms can help reduce the risk of sexually transmitted infections (STIs) that may lead to balanitis.
5. Regular Check-ups:
Visit your healthcare provider for regular check-ups to monitor and manage any potential risk factors or early signs of balanitis. This is particularly important if you have underlying health conditions like diabetes.
By following these preventive measures and maintaining good personal hygiene practices, individuals can reduce the risk of balanitis and enjoy better overall genital health. It’s also essential to seek medical attention if you notice any symptoms or suspect a potential issue to prevent the condition from worsening.
Conclusion
balanitis treatment is a vital aspect of managing this common genital condition, which can cause discomfort and affect a person’s quality of life. The approach to treatment depends on the underlying cause, which may include infections, skin conditions, allergies, or irritants.
Through proper hygiene, and addressing any underlying health conditions, individuals can effectively manage and treat balanitis. Seeking early medical attention and following a healthcare provider’s recommendations are key to alleviating symptoms, preventing complications, and improving overall genital health.
FAQs
Balanitis itself is not a sexually transmitted infection (STI), but the underlying infections or conditions that cause it may be contagious. Practicing safe sex and treating the underlying cause can help prevent transmission.
2. Is balanitis more common in older or younger men?
Balanitis can affect men of all ages, but it is more common in younger boys who may not have learned proper hygiene practices. However, it can occur in men of any age.
3. Can balanitis be a recurring condition, even after treatment?
Yes, balanitis can recur. Proper treatment, prevention measures, and addressing underlying health conditions are essential to minimize the risk of recurrence.
While proper hygiene and avoiding irritants are essential, it’s crucial to consult a healthcare professional for the most effective treatment. Natural remedies should be used with caution, as they may not be suitable for all cases and could worsen the condition.
CATEGORIES
- ACL Reconstruction
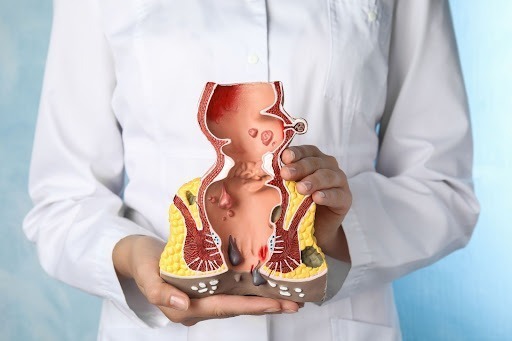
- Anal Fissures
- Anal Fistula
- Appendicitis
- ASK A DOCTOR
- Benign Prostatic Hyperplasia
- Breast Lump Excision
- Cataract
- Circumcision
- Conditions & Diseases
- Cosmetology
- Covid-19
- Cure
- Endocrinology
- ENGLISH VIDEOS
- Eye Care
- Gallstones
- General Surgeries
- Government Schemes
- Gynaecology
- Gynecomastia
- Health
- Health Insurance
- Hernia
- Hindi
- Hip Arthoscopy
- Hip Replacement
- Hip Replacement Surgery
- Hydrocele
- Kannada
- Kidney Stones
- Knee Arthroscopic
- Laparoscopic
- LASER
- Latest Treatments
- Lifestyle
- Liposuction
- Medfin Stories
- Medicine
- Nephrology
- Ophthalmology
- Orthopaedic
- Paraphimosis
- Patient Testimonials
- PCL Reconstruction
- Phimosis
- Piles (Hemorrhoids)
- Pilonidal Sinus
- Proctology
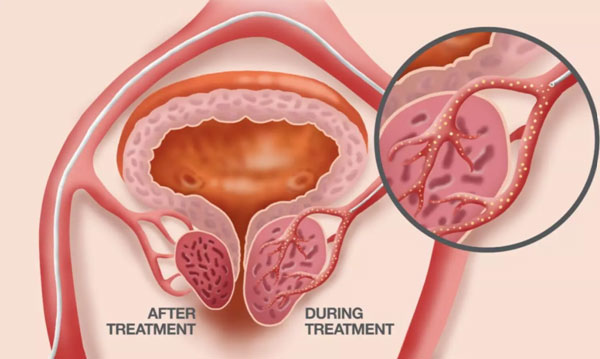
- Prostate Artery Embolization
- Rhinoplasty
- Second Opinion
- Total Knee Replacement
- Urology
- Uterine Artery Embolization
- Uterine Fibroids
- Varicocele
- Varicose Veins
- Vascular
- VIDEOS